The Peripheral Nervous System: Anatomy, Imbalance and Herbal Resilience
Welcome back to the Systematic Herbalism series. Previously, we explored the Central Nervous System—its tracts, commissures, and herbs that support cognition and spinal cord function. Now we turn to the peripheral nervous system (PNS), the web of nerves that links brain and spinal cord to every muscle, organ, and sensory receptor. Deeply intertwined with every system of the body, the PNS plays a vital role in our overall health. By understanding the PNS’s makeup—nerve fibers, ganglia, afferent and efferent pathways, as well as its two main branches—we’ll be better equipped to apply targeted herbal allies for nerve health, pain relief, and regeneration. That’s our starting point for this exploration.
Anatomy of the Peripheral Nervous System
To begin, lets go over some helpful terminology and how each piece works together to make up this powerful system. The peripheral nervous system is your body’s electrical lattice—an intricate weave of fibers transmitting sensory and motor messages between center and periphery. It is made up of bundles called nerve fibers that carry electrical signals between your central nervous system (CNS) and all the far-reaching areas of your body. These fibers are encased in protective sheaths, and they group together to form nerves, which travel through clusters called ganglia.
Ganglia are dense groupings of nerve cell bodies. Think of them as waystations where signals pause and organize before heading to their next destination—whether it’s interpreting sensory data or managing involuntary functions like digestion and heart rate.
The peripheral nervous system relies on two major types of pathways: afferent and efferent. Afferent fibers are like incoming messengers—they carry sensory information toward the central nervous system. They allow you to perceive texture, temperature shifts, and pain. In contrast, efferent fibers are the outgoing messengers—sending signals away from the CNS to trigger movement or activate glands. Think of it as a two-way street: afferent is the “input” lane, bringing in data from your body, while efferent is the “output” lane, delivering instructions back out.
To grasp this better lets look at an example! Say you brush your fingertip against something cool and smooth. That touch is detected by specialized receptors, which send a signal up through afferent fibers, passing through a dorsal root ganglion and onward to the spinal cord. In response, efferent fibers carry motor commands out through the ventral root, instructing your muscles to move—maybe to hold on tighter or let go.
Within the PNS, two overarching divisions govern every response: the somatic nervous system handles voluntary actions and conscious sensation, while the autonomic nervous system orchestrates involuntary processes like heartbeat, digestion, and glandular secretions. Another key difference lies in their physical targets: somatic neurons connect to skeletal muscle, while autonomic neurons reach smooth and cardiac muscle, along with the gastrointestinal tract.
1. The Somatic Nervous System
The somatic system is your body’s foundation for deliberate motion and sensory awareness.
Voluntary Movement: Motor neurons in the ventral roots send efferent signals from the spinal cord to skeletal muscles. Whether walking, writing, or petting a dog, these efferent fibers translate thought into action.
Sensory Processing: Afferent nerves collect input from mechanoreceptors (touch, pressure), thermoreceptors (temperature), and nociceptors (pain). These signals pass through dorsal root ganglia before streaming up neural tracts into the CNS for interpretation.
Reflex Arcs: Even without conscious thought, simple reflexes—like pulling your hand away from a hot surface—are mediated by somatic afferents synapsing directly with motor neurons in the spinal cord.
By bolstering myelin integrity and axonal health, specific botanicals can enhance both precision of movement and clarity of sensation throughout the somatic network.
2. The Autonomic Nervous System
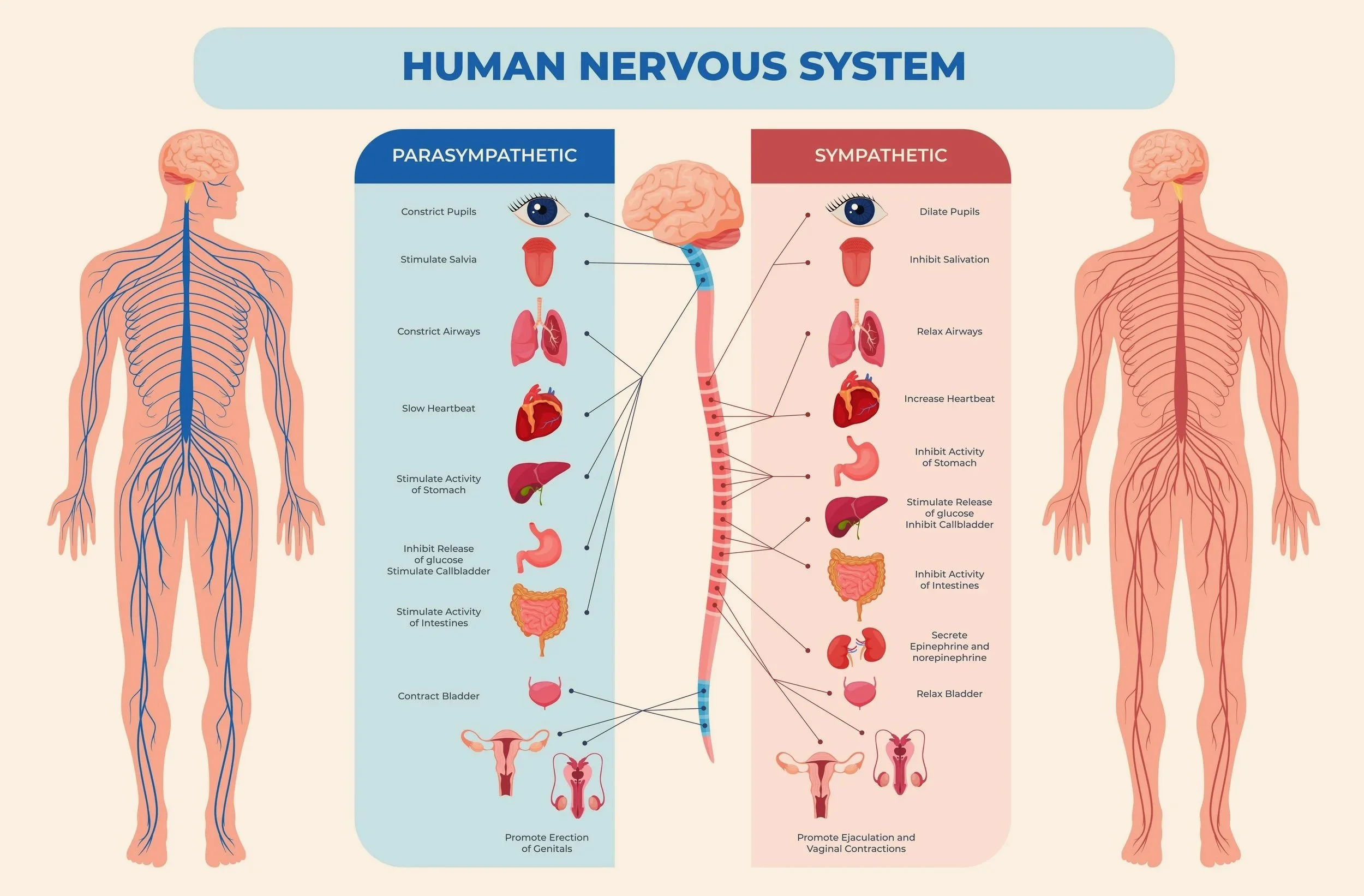
Operating largely beneath awareness, the autonomic system balances stress responses and restorative functions. It splits into two complementary branches, the sympathetic and parasympathetic. Maintaining dynamic balance between these two branches is vital.
2.1 Sympathetic Division (“Fight or Flight”)
Rapid Response: Preganglionic fibers exit the spinal cord, synapse in sympathetic chain ganglia, and dispatch efferent signals that increase heart rate, dilate airways, and mobilize energy reserves.
Neurotransmission: Norepinephrine released at postganglionic synapses readies the body for action—sharp vision, quick reflexes, and heightened alertness.
2.2 Parasympathetic Division (“Rest and Digest”)
Restoration Mode: Vagal nerve fibers and sacral outflows synapse in parasympathetic ganglia located near target organs, releasing acetylcholine to slow the heart, constrict pupils, and stimulate digestion.
Homeostasis: This branch governs energy conservation, smooth muscle tone in the gut, and glandular secretions for saliva and enzymes—all essential for repair and nutrient absorption.
To keep our bodies resilient and responsive, balance between the sympathetic and parasympathetic branches is essential. Overactivation of the sympathetic “fight or flight” mode can strain the adrenal and cardiovascular systems over time. On the other hand, a sluggish parasympathetic response may slow digestion and contribute to fatigue.
Imbalance in the Peripheral Nervous System
Peripheral nerve dysfunction can arise from trauma, metabolic disturbances (like diabetic neuropathy), infection, toxic exposure, or physical compression. When these nerves are impaired, their signals may be erratic, blocked, or misdirected. This manifests in conditions like peripheral neuropathy (burning, numbness, tingling), radiculopathy (radiating pain from compressed nerve roots), and autonomic irregularities (blood pressure swings, disrupted digestion, erratic temperature regulation). The result: reduced sensory clarity, compromised movement, and a decline in overall quality of life.
In the next section, we'll explore evidence-based botanicals that help recalibrate nervous tone—supporting somatic nerve repair, easing sympathetic overdrive, and enhancing parasympathetic stability.
Herbal Therapeutics for the Peripheral Nervous System
Botanical remedies can target the PNS through multiple actions: nourishing nerve structure, reducing inflammation, modulating pain signals, and promoting nerve regeneration. Below are evidence-based categories and exemplar herbs.
Nutritional Support and Neurotrophic Tonics
Evening primrose oil (Oenothera biennis) supplies gamma-linolenic acid (GLA), which bolsters myelin integrity and has shown benefit in diabetic neuropathy after 3–6 months of use.
Black cumin (Nigella sativa) offers thymoquinone, an anti-inflammatory compound that supports nerve health and reduces oxidative stress.
B-vitamin-rich herbs (e.g., nettle leaf, oat straw) complement dietary B-complex intake, essential for axonal maintenance and neurotransmitter synthesis.
Anti-Inflammatory and Analgesic Herbs
Turmeric (Curcuma longa): Curcumin inhibits pro-inflammatory cytokines and reduces neuropathic pain in rodent models and small clinical trials.
Boswellia (Boswellia serrata): Its boswellic acids suppress inflammatory pathways implicated in nerve irritation.
White willow bark (Salix alba): A source of salicin, it provides analgesia analogous to aspirin without synthetic processing.
Neuroregenerative and Neuroprotective Botanicals
Lion’s mane mushroom (Hericium erinaceus): Stimulates nerve growth factor (NGF) production, supporting axonal repair and improved nerve conduction.
St. John’s wort (Hypericum perforatum): Beyond mood support, hypericin and hyperforin promote nerve regeneration and attenuate pain signaling.
Gotu kola (Centella asiatica): Enhances collagen synthesis in peripheral nerves and protects against oxidative damage.
Topical and Local Nerve Care
Capsaicin (Capsicum annuum): Low-concentration creams desensitize pain receptors through substance P depletion, easing localized neuropathic pain.
Rosemary (Rosmarinus officinalis) and sage (Salvia officinalis): When used in compresses or infused oils, they improve circulation and deliver mild analgesia.
Calming Nervines for Nerve Pain Tension
Passionflower (Passiflora incarnata): Enhances GABAergic tone, reducing the emotional distress that often accompanies chronic nerve pain.
Modes of Administration
To support peripheral nerve resilience, combine internal tonics, anti-inflammatories, and regeneratives with topical applications and nervine teas or tinctures for stress relief. For example:
Morning: Take 1 g of evening primrose oil and a curcumin capsule with black pepper extract.
Midday: Sip a tea blend of nettle, oat straw, and lemon balm to maintain B-vitamin levels and calm nerve tension.
Evening: Apply a topical cream with muscle soothing herbs like comfrey or cedar.
Daily: Supplement with lion’s mane extract (500 mg twice daily) to foster nerve repair over weeks to months.
By tailoring dose and form—capsule, tea, tincture, topical oil—you can create a personalized peripheral nerve care plan. Always start with low doses, monitor response, and, if on medications or managing chronic conditions, consult a healthcare practitioner before beginning any new herbal regimen.
Harnessing these herbal allies empowers you to nourish, protect, and regenerate your peripheral nervous system—connecting mind, body, and spirit through the wisdom of plants.
Acupuncture & Peripheral Nerve Health
In addition to herbal medicine, acupuncture offers a promising modality for supporting peripheral nerve health. Rooted in traditional practice and increasingly backed by modern research, acupuncture can aid in pain relief, nerve repair, and autonomic balance.
How It Works
Acupuncture may stimulate nerve endings and trigger the release of neurochemicals like endorphins and serotonin, helping to modulate pain and inflammation.
Improved blood flow around affected nerves supports healing and tissue nourishment.
In some cases, techniques like electroacupuncture—gentle pulses delivered through acupuncture needles—have shown potential to enhance nerve regeneration and reduce hypersensitivity.
Acupuncture also helps balance the nervous system, calming sympathetic overdrive and strengthening parasympathetic tone.
Clinical Applications
Common conditions supported by acupuncture include:
Peripheral neuropathy from diabetes, chemotherapy, or injury
Radiculopathy caused by nerve root compression
Autonomic dysfunction (e.g., digestive issues, blood pressure swings)
Chronic nerve pain due to inflammation or trauma
Acupuncture works best when woven into a holistic approach. Paired with herbs, nutrition, and lifestyle support, it can amplify your care plan and deepen results. Treatment is individualized, so sessions are tailored to each person’s constitution and nerve-related symptoms.
As with any therapeutic practice, always consult with a qualified practitioner—especially when managing complex or chronic conditions. The synergy of acupuncture and botanical medicine offers a potent route to resilience: nurturing nerves from surface to center.
A Living Network Worth Nurturing
The peripheral nervous system is far more than a conduit—it’s a living interface between thought, sensation, and action. Whether translating the subtle texture of a leaf against your skin or regulating the silent rhythms of digestion, its quiet brilliance shapes every moment of embodied experience. By understanding this system’s intricate anatomy and functional dynamics, we unlock the ability to support it with intention.
Through evidence-based herbs—from trophorestoratives that rebuild nerve integrity to calming nervines that ease pain and tension—we can nourish the PNS at every level. The path to nerve resilience is not linear, but with botanical allies and conscious care, it becomes deeply personal and profoundly regenerative.
Your nerves speak the language of sensation and subtlety. Tuning into them—and tending them—offers a vital form of self-connection. In the next installment, we’ll dive deeper into formulation: crafting blends and rituals that sustain this essential system with wisdom, grace, and green medicine.
References
Timoszuk, Magdalena et al. “Evening Primrose (Oenothera biennis) Biological Activity Dependent on Chemical Composition.” Antioxidants (Basel, Switzerland) vol. 7,8 108. 14 Aug. 2018, doi:10.3390/antiox7080108
Hannan, Md Abdul et al. “Black Cumin (Nigella sativa L.): A Comprehensive Review on Phytochemistry, Health Benefits, Molecular Pharmacology, and Safety.” Nutrients vol. 13,6 1784. 24 May. 2021, doi:10.3390/nu13061784
Basu, Paramita et al. “Effects of Curcumin and Its Different Formulations in Preclinical and Clinical Studies of Peripheral Neuropathic and Postoperative Pain: A Comprehensive Review.” International journal of molecular sciences vol. 22,9 4666. 28 Apr. 2021, doi:10.3390/ijms22094666
Roy, Nand Kishor et al. “An Update on Pharmacological Potential of Boswellic Acids against Chronic Diseases.” International journal of molecular sciences vol. 20,17 4101. 22 Aug. 2019, doi:10.3390/ijms20174101
Lin, Chun-Ru et al. “Willow Bark (Salix spp.) Used for Pain Relief in Arthritis: A Meta-Analysis of Randomized Controlled Trials.” Life (Basel, Switzerland) vol. 13,10 2058. 14 Oct. 2023, doi:10.3390/life13102058
Szućko-Kociuba, Izabela et al. “Neurotrophic and Neuroprotective Effects of Hericium erinaceus.” International journal of molecular sciences vol. 24,21 15960. 3 Nov. 2023, doi:10.3390/ijms242115960
Klemow KM, Bartlow A, Crawford J, et al. Medical Attributes of St. John’s Wort (Hypericum perforatum) In: Benzie IFF, Wachtel-Galor S, editors. Herbal Medicine: Biomolecular and Clinical Aspects. 2nd edition. Boca Raton (FL): CRC Press/Taylor & Francis; 2011. Chapter 11. Available from: https://www.ncbi.nlm.nih.gov/books/NBK92750/
Gohil, Kashmira J et al. “Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all.” Indian journal of pharmaceutical sciences vol. 72,5 (2010): 546-56. doi:10.4103/0250-474X.78519
Anand, P, and K Bley. “Topical capsaicin for pain management: therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch.” British journal of anaesthesia vol. 107,4 (2011): 490-502. doi:10.1093/bja/aer260
Ghasemzadeh Rahbardar, Mahboobeh, and Hossein Hosseinzadeh. “Therapeutic effects of rosemary (Rosmarinus officinalis L.) and its active constituents on nervous system disorders.” Iranian journal of basic medical sciences vol. 23,9 (2020): 1100-1112. doi:10.22038/ijbms.2020.45269.10541
Aman, Urooj et al. “Passiflora incarnata attenuation of neuropathic allodynia and vulvodynia apropos GABA-ergic and opioidergic antinociceptive and behavioural mechanisms.” BMC complementary and alternative medicine vol. 16 77. 24 Feb. 2016, doi:10.1186/s12906-016-1048-6




















Hello and welcome! I'm Eve, a Chemist turned Herbalist, sharing the wonders of plant medicine and botanical skincare. Join me on this journey to Learn, Create, and Align your Divine!